In September 2014, a new study was presented in the USA. The aim of this comparative study was to compare the effectiveness of ultrasound-assisted needle lavage for the treatment of calcific tendonitis with shock wave therapy. The results of the study are clear according to rigorous scientific criteria. Ultrasound-assisted needle lavage for the treatment of calcific tendonitis is significantly superior to shock wave therapy.
Needle lavage leads to significantly better calcification removal than shock wave therapy. This led to reduced pain levels and significantly improved shoulder function for patients in the needle lavage treatment group.
This result is absolutely consistent with my experience with treating calcific tendonitis with needle lavage. In our practice, almost 3,000 patients had been treated with needle lavage by November 2014.
I regularly performed shock wave therapy myself until 2008. With the introduction of needle lavage, I increasingly abandoned shock wave therapy, as the results from needle lavage were more convincing in my hands. The new study confirms this feeling. It remains incomprehensible to me why needle lavage continues to lead a shadowy existence in Germany. With the ever-increasing number of positive studies, one gets the feeling that people in Germany want to ignore this therapy. Otherwise, the behavior of many colleagues cannot be explained when patients report how their doctor reacted when asked about it.
Study source:
As specialized as the diagnosis and treatment of shoulder injuries are, so are questions surrounding insurance law (professional liability insurance association law). Unfortunately, insurers often dismiss the consequences of shoulder accidents as pre-existing wear and tear, leaving the injured person at a disadvantage.
Especially in the case of the frequently occurring tears of shoulder tendons (e.g., tears of the supraspinatus tendon or subscapularis tendon), statutory accident insurance providers (professional liability insurance association BG) are particularly quick to reject claims. The result is a rejection notice.
As an expert witness for the social court, private insurers, and statutory accident insurance (employer's liability insurance associations, BG), I am confronted with legal questions every day. The often outdated level of knowledge surrounding various shoulder disorders and the consequences of accidents continues to shock me.
This lack of knowledge leads to accident consequences being rejected far too frequently, even though, based on current knowledge, many claims should be accepted. We often find that medical reports or BG statements submitted to us for assessment contain errors. In particular, lesions (tears) of the supraspinatus tendon or subscapularis tendon are incorrectly assessed based on current knowledge.
As part of this assessment service, we will first prepare a feasibility analysis for you.
We will review all available findings, expert opinions, accident descriptions, and other documents relating to your case. You will then receive an analysis, based on the most current state of knowledge, regarding the likelihood of success in your medical insurance claim. For this service, it is not necessary to visit us in person. Copies of your documents are absolutely sufficient.
If there is a reasonable likelihood of success, we are happy to prepare objection letters and corresponding detailed reports, with or without a thorough examination.
For the feasibility analysis, we are entitled to charge €101.99 plus VAT (total: €121.37). The calculation is based on the German Medical Fee Schedule (GOÄ) item 85, with a rate increase of 3.5. Detailed explanations for an objection or medical reports will be billed according to Section 85 of the German Medical Fee Schedule (GOÄ).


German international Sami Khedira is in top form for the Germany vs. Italy international match. But in the 67th minute, a challenge with Andrea Pirlo leads to a personal catastrophe.function-anterior-cruciate-ligament His right knee joint turns inwards. The 26-year-old immediately grabs his leg and collapses to the ground with a pained expression on his face. It's clear to presenters and viewers that something terrible has happened. A tear in the anterior cruciate ligament is a catastrophe for any athlete. Why is this ligament in the knee joint, which is only about 2.8 cm long, so important and why can injuries to the anterior cruciate ligament mean the end of an athlete's career.
The anterior cruciate ligament is the most important stabilizer in the knee joint. It is located in the center of the knee joint and is primarily responsible for preventing the lower leg from slipping forward relative to the thigh.
What many people don't consider is its function as a sensor. A healthy cruciate ligament contains numerous sensors for measuring tension and pull. This means that the tension in the ligament is constantly being measured, or how strongly it is being pulled. A nerve connection to the spinal cord can then reflexively control the muscles in the leg. Even before I consciously perceive a displacement in the knee joint, the cruciate ligament has already registered the dangerous condition. Via its nerve connection and the reflex circuit with the muscles in the leg, immediate countermeasures are taken, thus preventing anything worse from happening. This is also known as proprioception.
This makes the loss of the cruciate ligament doubly painful. On the one hand, the stabilizing ligament is missing, and on the other, the highly sensitive measuring device with its reflex circuit is also out of action.

The loss of proprioception in a cruciate ligament tear is also what often causes attempts at exclusive muscular stabilization to fail. Of course, a person with a cruciate ligament injury is capable of significantly building up their muscles to achieve improved knee joint stabilization. But without the sensitive cruciate ligament sensor and its reflex circuit via the spinal cord, muscular stabilization can only function to a limited extent. In most cases, there has already been significant displacement of the lower leg relative to the femur in the knee joint before the muscles even react. The knee is further damaged. This makes surgery unavoidable for athletically active individuals. Since suturing the anterior cruciate ligament unfortunately does not work, various techniques for replacing the anterior cruciate ligament have been established. Two different transplants are most commonly used today: the patellar tendon or semitendinosus tendon, together with the gracillis tendon, two tendons from the posterior thigh. Both procedures have their advantages and disadvantages.

Here are a few bare figures on the mechanics of the cruciate ligament and the most common transplants:knee mri A healthy cruciate ligament has a tensile strength of approximately 2160 N. That corresponds to approximately 220 kg. The tensile strength of a patellar tendon transplant is between 2400 and 3600 N, depending on the selected width. The tendons from the posterior thigh are even stronger. A quadruple graft made from the semitendinosus and gracillis tendons has a tensile strength of over 4100 N. That corresponds to more than 410 kg. Since the transplants themselves are all significantly more stable than the natural cruciate ligament to begin with, the weak point of the system is not the transplant, but the attachment of the new ligament to the bone. A variety of different implants are available for this. All of these screws, plates, or pins are intended to hold the tendon in the bone. They do just that, some more than others.
Ultimately, however, there is no other option than to give the transplant sufficient time to properly grow into the bone.
This is where the patellar tendon graft demonstrates perhaps its only real advantage over semitendinosus and gracillis tendon grafts. Due to the bone fragments present in the patellar tendon, it integrates much faster into the bone and is often firmly integrated after just 6-12 weeks.
Let's get back to Sami Khedira. The very next day, the media reported a downtime of approximately six months. Why six months, when such a transplant heals in 12 weeks? The magic word is "ligamentization." When the transplant is removed, all the blood vessels that supplied it are severed. It is taken from the body and implanted in a completely different location. This severing of all the blood vessels always causes a cruciate ligament transplant to initially partially die.
All readers who were pleased in the previous section about the high tensile strength of the transplants compared to a natural cruciate ligament should be aware that the transplant does not remain as stable. Due to partial death, the transplant loses a considerable amount of tensile strength. This can even decrease to the point where the tensile strength of the transplant is temporarily significantly lower than that of a healthy cruciate ligament. Then the process of ligamentization begins. This means that the former tendon is converted into a ligament - the anterior cruciate ligament. First, new blood vessels are formed. Then connective tissue cells, so-called fibroblasts, migrate into the tendon transplant. These fibroblasts then begin a continuous modification of the collagen structure of the transplant. This slow remodeling process, in which the tendon is transformed into a ligament, is also known as remodeling.
In the first six weeks after surgery, there is a significant decrease in tensile strength. Only then does the transplant slowly stabilize and regain strength. Studies have shown that this ligamentization process takes at least a year. There is currently no way to accelerate this process. Even the best physiotherapy, which Sami Khedira will certainly receive, has no influence on the ligament's phased healing behavior. Many experts assume that after about six to eight months, the new ligament will have reached the tensile strength of a healthy cruciate ligament. Unfortunately, there is no guarantee of this. For this reason, all recreational athletes are advised to refrain from all high-risk sports for at least a year after cruciate ligament surgery. However, the pressure on our professional athletes is so immense that they often return to their sport much sooner. Unfortunately, this repeatedly leads to serious setbacks, as the long list of footballers with recurrent cruciate ligament tears demonstrates.
I wish Sami Khedira all the best on his recovery and that he will soon be able to play for the German national team again.

When patients are asked what quality means in medicine, the answers vary widely. They often mention things like friendliness, waiting times, or waiting room amenities. From a medical perspective, however, the aforementioned criteria have no influence on the quality of treatment. Even review portals cannot reflect this quality. The quality of medical treatment or diagnostics is very difficult for laypeople to assess. It is made up of many components. Technical equipment, professional competence, and care are certainly among them. In recent years, health insurance companies and the Association of Statutory Health Insurance Physicians have been trying to improve the quality of diagnostics and medical therapy. For this reason, verifiable quality criteria for ultrasound examinations were introduced in orthopedics in 2009. This affects, for example, the quality assurance agreement for infant hip replacement. This agreement stipulates a minimum standard of technical equipment and relies on a high level of professional skill that leads to reproducible results. The aim, for example, is to remove ultrasound devices from circulation that are so poor or old that diagnostics are only inadequately possible.

Over the past five years, the number of orthopedic practices in Saarland that offer ultrasound diagnostics, for example, for infant hips, has shrunk from over 50 to 19. Instead of modernizing technology or improving quality, they often choose not to provide ultrasound services at all. This is despite the fact that ultrasound examinations now play an integral role in the diagnosis of many medical conditions.
It plays a significant role in the diagnosis of many medical conditions. From the very beginning, we have strived to offer our patients high-quality ultrasound diagnostics. Compared to other procedures, ultrasound examinations offer an unparalleled ability to quickly and reliably visualize diseases in images, and are completely radiation-free. We currently have two modern ultrasound machines that far exceed the requirements. Our patients can be assured that we will continue to strive for quality and modernize technology in the future.
Many colleagues in orthopedics view our specialization in the shoulder joint with skepticism. Why further specialize when you already specialize in the field of orthopedics?
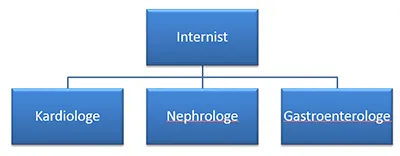
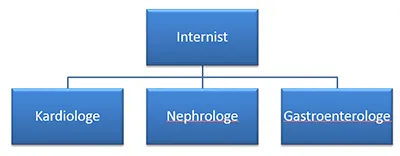
Other medical specialties had already embarked on this path years ago, and today no one questions the wisdom or nonsense of this specialization. Scientific progress simply made it necessary. Internists are a prime example. While initially there was only one internist, knowledge quickly increased so rapidly that individual doctors were overwhelmed. It became unavoidable to specialize in various organs, and today, usually only in one organ. Today, no one would question the necessity of specializing as a cardiologist, nephrologist, or gastroenterologist.
Our theoretical knowledge in orthopedics is also constantly growing. In addition, operations are becoming more and more specialized and many things that were considered impossible years ago are now standard. The development that has already largely taken place among internists has also found its way into orthopedics some time ago. It is criminal not to recognize this development and to continue to claim to be "up to date" in all areas. I dare say that this "universal specialization" is no longer possible in orthopedics today. Unfortunately, there are still too many doctors who consider themselves to be universal geniuses. Whether they always act in the best interests of the patient is something each individual must answer for themselves. Fortunately, some colleagues have already recognized this development. Similar to the specialization of internists in one organ, there are an increasing number of orthopedists who specialize in a particular joint. I recognized this need for specialization back in 2006 and focused my interest on shoulder disorders. Extensive continuing education and constant engagement with the subject matter were necessary to get to where we are today. Additionally, significant investments in ultrasound technology, X-rays, and surgical instruments were necessary to be able to offer specialized diagnostics and treatment from a single source. Today, I can rightfully claim that our practice is a center for the diagnosis and treatment of shoulder disorders.