For anyone who has always wanted to know how arthroscopic refixation of a supraspinatus tendon works, I have posted a photo gallery with comprehensive explanations online.
We now know that a torn or ruptured shoulder tendon unfortunately cannot heal on its own. Even intensive exercise is unable to heal the tendon. While the symptoms can often be managed well with conservative therapy, the tear does not heal!
Over time, tendon tears in the shoulder become increasingly larger.
We have been performing needle lavage routinely to treat calcific tendonitis for more than 10 years. During this time, we have continually perfected the technique. Today, we are faster and more gentle than just a few years ago.
The recently published major international studies prove us right. Needle lavage for treating calcific tendonitis is the most effective procedure, with minimal risk.
Nevertheless, patients are often confused by claims that their calcification is much too large or too hard for needle lavage.
These statements are simply false!
The image shows the X-ray of a patient before and after calcific tendonitis treatment in our practice. This patient's calcification was not large, but gigantic!
Our experience over the past 10 years shows that there are no calcifications too large for needle lavage. We also almost never experienced anything too harsh; this happened perhaps in one out of 1,000 cases.
Our new video on impingement syndrome is currently in the works. I've been thinking a lot about this new episode of our video blog over the past few weeks.
Surgery for impingement syndrome is still performed far too frequently, even though it's known that reaming the acromion rarely solves the problem.
A painful shoulder combined with restricted movement is not uncommon. Many diseases can be responsible for these symptoms.
If the restricted movement continues to increase, however, it could be frozen shoulder – also known as a frozen shoulder or simply shoulder stiffness. This phenomenon is a distinct clinical picture.
We are currently scouring our medical records and scientifically evaluating the results. Even today, there is little data on frozen shoulder. Many studies contain only a few cases and are therefore inaccurate. Over the past five years, more than 2,000 patients with this diagnosis have been treated in our practice – a significant number.
In addition to the latest scientific findings, our personal experience in treating these more than 2,000 cases also influences our diagnosis and treatment decisions. This is an invaluable wealth of knowledge that benefits our patients.
The first result of our own analysis is the age and gender distribution of these 2,000 patients.
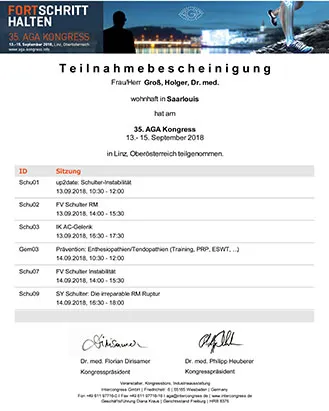
As every year, a variety of conferences and continuing education events take place after the summer holidays. A special highlight is certainly the AGA Congress. At the annual congress of the Society for Arthroscopy and Joint Surgery, the latest findings and therapies are always presented and, above all, discussed among experts. This year, the event took place in Linz, Upper Austria. Although the journey was somewhat arduous, my participation was rewarded with new knowledge.
New doesn't always mean better. However, this year, several things were discussed in the shoulder area that will influence my treatment decisions.
There is a great deal of knowledge available, particularly regarding instability following joint dislocation (joint dislocation). While in the past a simple MRI scan was often sufficient to make the diagnosis and determine the indication for surgery, today specialists recommend a much more differentiated approach. In addition to X-rays, a 3D CT scan is particularly useful in many cases in order to plan the correct surgical procedure. Why all this effort? In most hospitals, planning and decisions are only made based on MRI. The question is easy to answer. But the new studies show that the bony situation of the acetabulum and humeral head often determines the success or failure of a treatment. We want to minimize the risk of surgical failure and thus new dislocations.
Another notable piece of news is that hyaluronic acid has a positive effect on tendon healing. This has been assumed for some time, but now it's been proven. This, too, will change our treatment regimen. In the future, patients with tendon injuries, especially after shoulder surgery with tendon sutures, will also be able to choose this additional therapy.